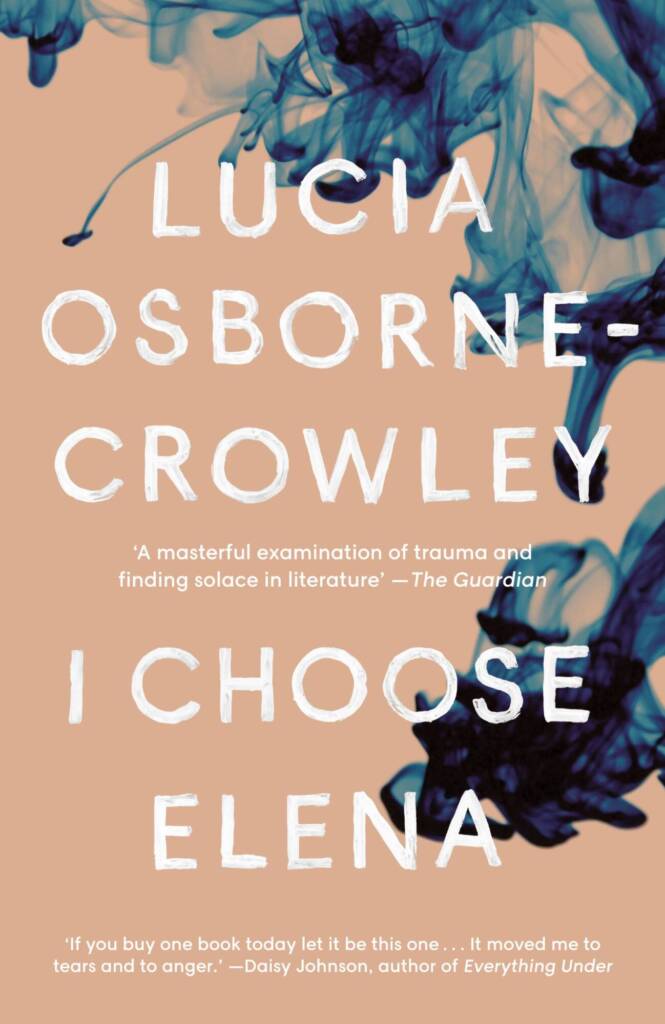
Interview of Lucia Osborne-Crowley by Freya Bennett
It was a rainy Wednesday in an alternate universe when I drove through the downpour to meet Lucia Osborne-Crowley at my favourite café. The traffic was bumper to bumper and I accidentally drove through a red light, misjudging the timing. I would later get a $400 fine.
I was worried about being late for our interview but I should’ve realised that if I was stuck in traffic, the likelihood would be that she was too.
I arrived at the café just on time but received a lovely message on Instagram from Lucia that she was running late. PHEW! I had time to prepare some questions. I was in the middle of moving house with a toddler and hadn’t had a moment to sit down and formulate any cohesive thoughts about how much I loved her book ‘I choose Elena’.
How does one ask questions, in a café, about a book that deals with rape, trauma, and lifelong chronic pain? Once I delved back into the book again, I jotted down so many questions that I had to stop myself. This book was eye opening, life changing and so perfectly written that I couldn’t wait to meet the author.
Lucia arrived, her smile warm and relaxed. I had a feeling we would get on from reading her book and following her Instagram and I was so relieved to see my prediction was true. We had a chat about astrology and coffee before realising we only had 30 minutes to run the interview – Lucia had to be at the airport as she was midway through her book tour.
We ordered coffee and began our chat. The book is so without fluff that I decided to delve straight in to the hard stuff.
F: How was it writing a book that deals with something so deeply personal and traumatic?
L: (Lucia laughs)
It was very hard. And I laugh when I say that, because I underestimated just how hard it would be. I had published an essay in June of 2018, which was then commissioned to be turned into a book and there was a long process of me deciding whether or not to publish that first essay.
Before the essay, I had just started telling my doctors about the assault that had happened years ago, which lead me down the path of getting all of this really specialised care. I was seeing all these physical therapists and going to physical rehab, which is incredibly lucky. It was amazing how this whole world opened up to me as soon as I told one person about what happened to me.
And then because it was all very emotionally overwhelming, I just pretended I was working and reporting a story about someone else. After ten years of saying nothing I was then waking up every day and going over it and over it and over it and I just couldn’t do it. So I took my notebook in every day and just pretended I was working as a journalist. In my first job as a journalist I reported almost exclusively on sexual violence and domestic violence – I was a gender reporter and so it was quite easy for me to pretend I was working. I would go into these appointments and pretend I was interviewing the doctors when in fact, I was in my own appointments.
Did they know you were doing that?
Yes. I would be like ‘so, if a person did blah blah blah,’ and they would be like ‘yes,’ going along with it. But it was purely a cooping mechanism. I came to the end of it and I was looking around the room, the journalist in me wanting to say ‘Is anyone else hearing this? This is wild!’ I had no idea how strong the connection was between rape and sexual assault and long term illness – physical , psychological and emotional.
This information really changed my life, potentially saved my life and it was only available to me because I am lucky and very privileged. I had a job in a law firm so I had enough disposable income to see these specialists. Our public healthcare system is great but it doesn’t cover the kind of people I was seeing.
I came to the end {of the treatment} and I had hundreds of little pages of notes I had written down. And I thought, I think that people should know about this. Journalism has always been a way, in my mind, to get information out there that there are otherwise structural barriers to getting. At first I was like, maybe I should publish this as I was pretending it was, as a story of someone else. And then I considered publishing it under a pseudonym but I had spent months and months working with these doctors who had helped me understand that this is not a shameful thing and that I did nothing wrong, and I really believed it by this stage so I couldn’t marry that with publishing under a pseudonym. Either I’m ready to publish it or not. That’s not to say that publishing things pseudonymously is not also a really powerful thing to do but I just thought, after all the work I had done, I would like to publish this under my own name.
Where was the article published?
The Lifted Brow and also on the ABC in a very different form. So there were two very different versions, the same story, published on the same day.
Quite quickly after that I was commissioned to turn it in to a book by a publisher in the UK and because the process of publishing the essay was quite full on and took me a while to recover from, for some reason, I was just full of confidence that it would be fine, that the hard part was over? And I was wrong. Your brain does a funny thing when you’re trying to do something that’s going to be really hard, it gives you these false milestones where you’re like ‘ok, now I’ve done the hard part,’ even though the worst part was definitely still yet to come. I think if I had known how hard it was going to be, I wouldn’t have done it. I wasn’t brave at all. I was naïve.
I think that’s such a human thing, otherwise we wouldn’t do anything.
Exactly.
Well, I’m glad you thought it was going to be easy, because this book is so amazing. I’m really interested in the topic of pain as someone who has experienced acute pain, but not chronic pain and how the medical profession treats pain on a holistic level. And also women’s pain and the difference in treatment and belief that goes on. What are your thoughts on pain, and what do you feel about pain after writing this?
It’s such a great question and I too am fascinated by pain. Because, for the ten years I was experiencing acute and chronic pain, I was in and out of hospital and my diagnoses was very unclear, I had a really antagonistic relationship with pain. The messages I was getting, was that I should be able to bear it. But I couldn’t, I really couldn’t. And that created a huge amount of conflict in my mind because I wanted to be someone who could, desperately.
I’d always considered myself to be stoic; you know, all these things I now know aren’t that inherently valuable, but I was brought up to think they were. So it devastated me that I was succumbing to pain, especially when I could see that everyone around me wanted me to stop succumbing to it. I kept having these experiences with doctors where I could see in their faces and in their body language, hear in their voices that it would be so much easier for them, if I could just handle the pain.
Pain is subjectively experienced and we don’t yet have a way to measure it, which means not only are we reliant on how credible the doctor sees you as a person (and that statistically depends on whether or not you’re a woman or a person of colour) but because it’s subjective, there’s this strange idea that we can control it. Which is not how pain works and more than other physical symptoms pain exists in the brain and in the nervous system in a way that means it can persist even when a physical injury has resolved itself. So it’s actually one of the more persistent physical symptoms a person can experience.
And that must be so hard, especially as a woman or a minority because we are taught from early on to make everyone feel as comfortable as possible even if that means ignoring our discomfort.
Exactly and the people pleaser in me just wanted so badly to make it go away and I was being made to feel I had the power to do that, whereas other patients aren’t made to feel that way. The other thing with pain is that because it’s self reported the doctors can choose based on how sincere they think you are, how to treat it. For example, studies show that if men and women come in to an emergency room, reporting the same amount of pain on the 1-10 scale, the woman will wait significantly longer than the man reporting the same level of pain and will also will be treated with a much lower dose of pain-killers. And the assumption underlying that, is that a woman’s pain is exaggerated and a man’s pain is actually what he reports it to be.
And for communities of colour, the gap is even wider. They’re 22% less likely to be seen as quickly and the difference in dosage is much wider, not only because of the credibility problem, but because doctors have a bias about opioid addiction.
Wow! I knew this at a very basic level but I think for people who haven’t experience persistent, chronic pain, this would be astonishing. Can you talk to me more about how pain can become an illness on it’s own?
There was a really great article in the National Geographic about pain and how it becomes a disease in it’s own right and doctors are not really across this. I’ve met very few doctors that understand that pain can become a pathology. It can become something that stands alone and can exist completely separately from accident or injury. And that is a neurological disorder and we treat other neurological disorders very seriously. I read yesterday when I was following up on studies from the book that 85% of people who have chronic pain conditions are women. And that’s a combination of things like endo, fibromyalgia and pain resulting from illnesses that disproportionately effect women. I refuse to believe there is not a connection between that and the fact that chronic pain isn’t taken very seriously.
And the weird thing about not believing women’s pain is that we are made to give birth, we are made to handle intense pain.
This is the thing, studies show that women’s pain threshold is much higher than men’s even though the assumption is so often the opposite. Masculinity is associated with stoicism so people think that if men come to an emergency room saying ‘I’m in pain’ then they must REALLY be in pain when in fact the opposite is true. Women are much less likely to get help for pain until it’s really really bad. Whereas men, are much more likely to get help for lower levels of pain. Pain really freaks them out and we are much better at it. And the thing with the 1-10 scale is that we all put our experience in to a narrative and everything is relative. And because many women go through childbirth, they then have that as the highest level of pain on their scale whereas men have nothing like that to compare on their scale.
You talk a lot about the specialists you saw in your book and how mainstream medicine can often use a bandaid approach instead of getting to the root cause, what do you hope becomes more mainstream as we learn more about trauma and pain?
I really really hope we embrace that holistic stuff more because when we understand pain a bit more, we understand a lot of it is neurological. This means there are so many different ways to approach and help ease the pain. There are so many connections {when it comes to neurological pain} that if you find a way to relax the muscles then the parts of the brain that are reinforcing the pain signals will also relax. And you can do it the other way round too, so if you try and relax the nervous system, then the muscles which are tightening in response to the pain signals will also relax. That’s why the holistic path is so important too. And I didn’t understand that for so long, but especially if you have a pain condition and an inflammatory condition {like me}, if you get into habits that relax your nervous system, calm your anxiety and relax your muscles, then you can manage pain a lot better. So for me, I get massages twice a week and I meditate and do yoga everyday. In the past, I scoffed at that stuff. I was in so much pain I just thought I needed serious medical intervention, and I have that too. My endo is managed by surgery and my crohns is managed by steroids and immunosuppressants but the other stuff really helps too. It’s so important.
And because it’s scoffed at so much, people think it’s really cool to hate natural medicine.
Exactly, when in fact it’s been lifesaving for me. And it just helps take the edge off. And I would never say to anyone with any kind of chronic pain condition that it’s enough, but it helps so much.
So in terms of support, how can I be an ally to someone experiencing chronic pain? What has been the most valuable support you have received?
That’s a great question and something I want to talk about more actually. I think it’s a lot about listening, that’s the main thing. And it’s a lot about offering explicit signs of belief. Leslie Jamieson writes about this a lot, that you can express empathy and understanding but it’s also really important to voice it.
To say I can see that you’re in pain or I can see that you’re suffering is really really helpful. And keep in mind agency, give a sick person that in any way that you can. Practical stuff is also really really helpful. I have friends who will just bring over pasta and say you can have this now and I’ve made this to go in to the freezer. And I just don’t have to ask, because that’s really hard.
Doing things without being asked is really helpful and something I appreciate a lot. Having someone who understands I can’t necessarily talk or engage and will just drop food over is amazing.
We then realise Lucia’s taxi is waiting to whisk her away on an adventure we can only dream of now, and as much as I could talk about this topic and her vast knowledge for hours, we have to leave it there.
You can buy I choose Elena here.