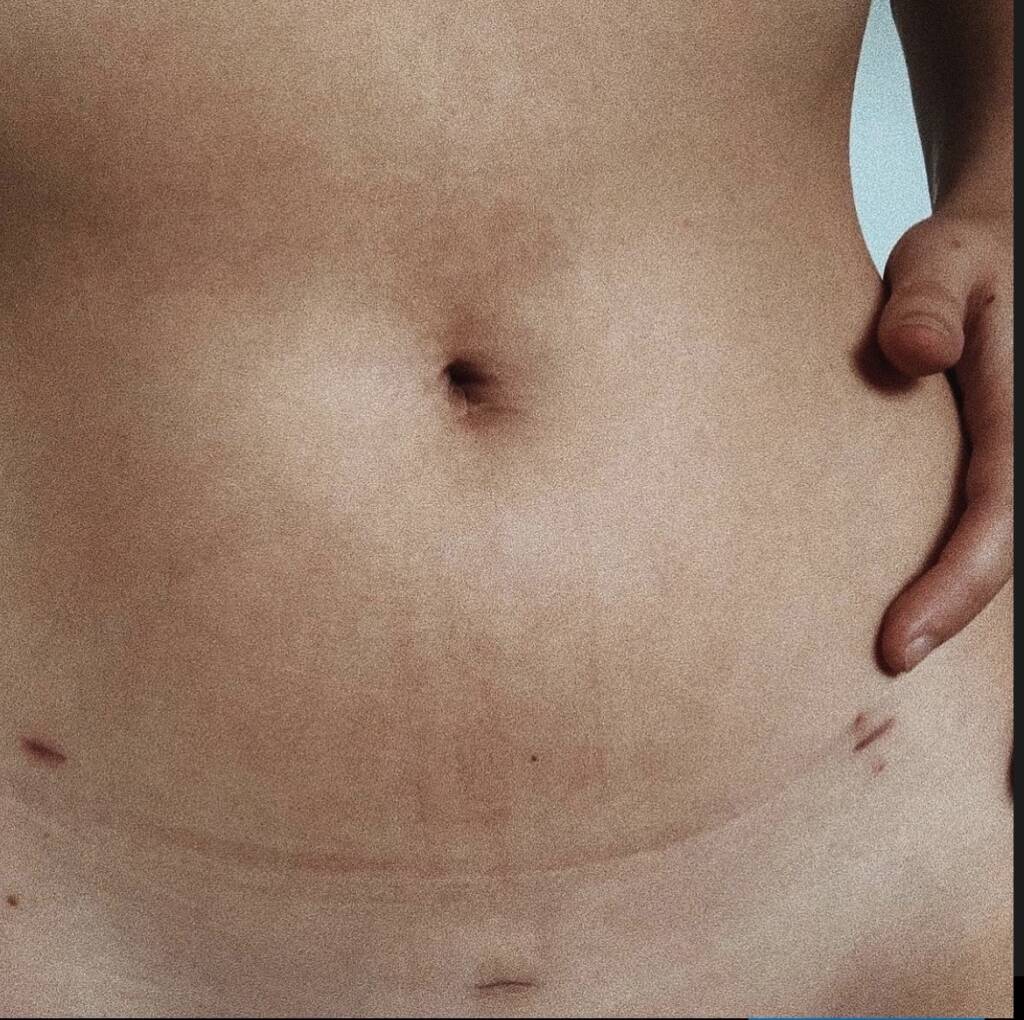
Writing by Haylee Penfold // photograph by Blitzed Images
 March is Endometriosis Awareness Month. In Australia endometriosis affects at least one in 9 girls and women and those assigned female at birth.
March is Endometriosis Awareness Month. In Australia endometriosis affects at least one in 9 girls and women and those assigned female at birth.
Shockingly, on average it takes up to nine years to receive a diagnosis of endometriosis. Even then, there is no cure for this disease and most gynaecologists aren’t trained on proper surgical treatment. While the topic of endo is gaining more attention – with $58 million of government funding going towards treatment – there is little being done to address a core issue amongst the way these people experiencing pain are being treated.
Here is my story.
I am just one of the thousands that highlight the issue of misogyny in how women and people with a uterus face gaslighting, belittlement and dismissal of their symptoms and experiences while seeking medical advice and treatment for their pain.
When I started getting my period, I was in my first year of high school. It didn’t take long to notice something was off. My week of bleeding was violent. I would struggle to sleep, my bleeding was heavy and I would feel nauseous from pain. My peers would question why I was missing school because of my period and I didn’t really have an answer for them.
During those years in school, I lined my underwear with three overnight pads, my best attempt to prevent leaking blood onto my skirt. Sometimes it worked, though oftentimes it didn’t.
My mum took me to the doctors when I started missing more school. She grew concerned because I was beginning to faint from the pain my period was causing. The days I was bleeding I had barely enough energy to get out of bed. My family doctor was a male, he had always been helpful with my asthma and other childhood or seasonal illnesses. When my mum brought up my period, his demeanour changed. Before I could even begin to explain how bad my pain was, he cut me off.
“You’re a young woman, this is exciting. These things can happen, often they figure themselves out. Just give it time.” and that was it.
It took another twelve months of intense pain and seeking another doctor for someone to at least listen to my symptoms. This time a woman. I was thirteen when I was put on the birth control pill. She explained to me that it would help regulate my period and hopefully slow down the bleeding. Though, eventually I learnt that it does nothing of the sorts. Within weeks I was met with the abundance of side effects that came with this little white pill. Again though, my pain was never addressed.
It wasn’t until I was seventeen, five years after my pain had started that I was referred to a gynaecologist. It took me mentioning that I had become sexually active and experienced pain during intercourse to get a red flag put on my case notes. By this time, I’d done my own research and familiarised myself with the basics of PCOS and endometriosis. I wanted answers, not just a band-aid solution that birth control had provided.
The gynaecologist doubted that I had either condition, I was told again these things happen and eventually they would sort themselves out. She told me that to be diagnosed with endometriosis I’d need to have surgery. So she offered a more invasive kind of birth control – an IUD to be inserted inside my uterus – as a solution. All I heard was another band-aid. I shook my head and with tears falling I begged. I begged her to do the surgery so at least I could cross endometriosis off the list of possibilities and be one step closer to an answer for my pain. With hesitation, she agreed.
I woke up from that surgery so nervous. Still groggy from the anaesthetic and the nurse told me it all went great and that the gynaecologist would see me soon to tell me the results. It was a bittersweet moment when she came. She rubbed my arm and told me the news.
“You have endometriosis. We found it on your bowel, bladder, pouch of douglas, left ovary…” she said.
Ironically, it was after my diagnosis that things really went south. I felt better… for about three months. The advice I’d gotten was to take panadol for my pain and go back to see her when the pain got bad again. I did more research and took notes like a medical student would. I learnt that there are ways to surgically treat endometriosis. You can either use methods of excision or ablation. Excision has been proven to be more beneficial for long term treatments of endometriosis, though looking through my surgery notes of what I’d had, I read the word ablation. To compare the two, ablation lasers the superficial endometriosis but fails to remove the disease that is deep into tissue of organs that excision can.
I’d been in and out of hospital for months, waiting in the ED, crippled with pain. The hesitation to seek help grew with each experience of care from doctors. While being treated in hospitals at my most vulnerable state, I’d been accused of being addicted to opioids, that I was putting on an act to get more pills. I had sometimes even requested a female doctor in the hopes they’d be a little more understanding, even then, I’d been told “it’s just a bad period”.
From there, I reached out to another surgeon in my area after reading that he referred to himself as a “specialist in endometriosis care”. I told him my story and within six months I was on the operating table again with the reassurance that this surgeon knew the difference between ablation and excision, that I’d be in better hands.
I woke up and again, the person I’d trusted my body with – to open me up and fix me, had let me down. I asked where it was, where the endometriosis had grown. He laughed at me. Told me there was nothing of the sorts. That it had all been a misdiagnosis.
“Have you had an STD test? I think you have chlamydia and have for a while” he said with a smirk on his face. He stood above me with his hands crossed over his chest. My cheeks burned as he spoke the words almost too loudly.
I told him that couldn’t be possible. That I’d been tested after every partner and nothing ever came back positive. He told me that he opened me up and that everything was so inflamed that it pointed towards a condition associated with long term chlamydia. He referred me to a pain specialist to assist me with the management of my pain and told me to ask my GP about how to address the chlamydia.
When I spoke to my GP, I told her how he had made me feel that day after surgery. Being laughed at and humiliated was something no patient should ever have to endure from a medical professional. We agreed to not go back to him, and that maybe the pain specialist referral could be the silver lining of the terrible experience.
With hopes that the pain specialist could assist me in treating my pain, I took my fiance to this appointment as support. From pictures, I’d grasped that the appointment was with a male but I pushed down my reservations from past experiences and hoped for the best. Within the first five minutes of my time in his small office he referred to me as “another woman with endometriosis”. He asked me what makes my pain worse, I told him my period, stress, exercise and sex. It was then that he looked at my partner, (also a male) and back at me.
“You’re lucky that he sticks around through all this, it has to be hard for him too.” he said, praising my fiance. He failed to address my pain and suffering, even though it was the reason we were in his office, paying almost $400.
Fast forward two years and I finally found the specialist I needed. The almost three hour drive into Sydney was more than worthwhile to receive appropriate treatment.
“I hear you, and see you and believe you. We are going to figure this out,” he said, and I burst into tears because I believed him.
He went beyond proving himself. He told me there are four stages of endometriosis, varying in severity and I had the most severe. My pain was validated and he didn’t give me any band-aids. He offered real solutions and options and choices that I’d never been given before.
Almost ten surgeries later here I am. Finally, being heard.
I am 25 years old and only now am I in a place where I feel confident in how my health is being treated. I have stage four endometriosis, a case so severe I’ve needed surgeries every six months to treat adhesions on my organs.
My focus now lies on my fertility, and seeking support with IVF clinics. It’s hard not to get angry, that maybe if I was saved all those years ago instead of the health system failing me, I would have more time, more opportunity to fall pregnant on my own?
$58 million can do so much.
We need to start with educating medical professionals of what this disease is and how it presents itself.
We need to have doctors begin the investigation with the thirteen year old who is missing school because her period is so painful she faints, not the twenty five year old who can’t fall pregnant or who can’t have intercourse due to the pain.
Instead of insisting young women go on the pill to hide the symptoms, why not focus on the root cause? 1 in 9 women are suffering because misogyny is so deeply rooted into the healthcare system that it is failing them.
Sign the petition to change the treatment guidelines here.






